*/

On St Patrick’s Day morning this year, our youngest coughed. She coughed again. On high alert, we began a period of 14 days’ isolation during which the country was locked down. My practice, as a clinical negligence barrister, moved from being largely chambers-based to my study at home.
In spite of lockdown, and unlike colleagues in other areas of the law, I was able to continue my practice largely without interruption. Few clinical negligence cases go to trial and almost all other stages of the litigation – from the barrister’s point of view – can be dealt with remotely. Mediations and settlement meetings, in particular, seem just as successful conducted on a virtual platform.
However, many clinical negligence claims at an early stage in Spring 2020 are now subject to delay since medico-legal examinations have been difficult to organise and domiciliary visits necessarily had to be suspended during lockdown.
Claimant and defendant lawyers have largely cooperated and adopted a sensible and pragmatic approach to the challenges they face: on 14 August 2020 a new protocol was finalised between NHS Resolution, the Society of Clinical Injury Lawyers and the charity AvMA which agreed, among other things, moratoria on limitation periods until three months after the protocol ends.
Aside from the practicalities of running an existing clinical negligence claim, what are the wider implications of COVID for future clinical negligence litigation? Will there be claims by those who have contracted COVID? Probably, although the majority will likely be personal injury claims, especially employer’s liability claims for failing to provide a safe work environment and, in particular, a failure to provide adequate PPE.
Some patients may seek to bring claims against medical institutions where they have contracted COVID. In September 2020 University Hospitals Bristol and Weston NHS Foundation Trust published the findings of its investigation into a cluster of COVID deaths at Weston Hospital. The Trust apologised to the families of the 18 patients whose deaths ‘may’ have been avoided. Breach of duty in these cases may not be difficult to prove, but causation will surely be more complex, since claimants will have to prove where and how they contracted COVID and, in a fatal case, whether COVID was the cause of death. This would likely involve expert evidence from virologists and epidemiologists and, in an adversarial system, causation could be problematic (although one could imagine the doctrine of ‘material contribution’ having a role to play in some such cases).
Some of the litigation which, in the early stage of the pandemic, caused significant anxiety amongst healthcare professionals concerned the ethics of decision-making. There was a fear that doctors would be sued for their life-or-death decisions over who got a ventilator and who didn’t. Such cases would be difficult to pursue. It is a defence to a clinical negligence claim to have acted as a responsible body of your discipline would have done. So provided the actions represented those of a reasonable, responsible body of medicine and the decision-making was not illogical, there would be a defence. The courts would also, I consider, bear in mind the agony of such decision-making in a time of crisis.
It was precisely the anxiety about such claims which led to the MDU’s call, in the early days of the pandemic, for blanket immunity from clinical negligence claims for doctors in COVID times (and some US states have enacted exactly such provisions) but at present there is no indication of such legislation being enacted in the UK.
The real impact of COVID on clinical negligence claims will be on the standard of care.
Clinical negligence claims depend on the claimant proving that the relevant practitioner has fallen below a reasonable standard. It is not just doctors who owe their patients such a duty: all those involved in the running of a medical institution, from hospital porters to chief executives, have to take care when undertaking their role.
While COVID does not affect the existence of the duty, it does – and may fundamentally – affect the standard of care. This, in turn, could mean that some cases of clinical negligence are more difficult to prosecute.
In some cases the standard of care will remain unaffected: the skill with which an elective podiatry procedure is performed is likely to be judged to a similar standard in a COVID and a non-COVID world. However, emergency surgery may be affected where a hospital has COVID patients and resources have had to be diverted. In June of this year my son had appendicitis. The surgeon at Manchester Children’s Hospital (whose staff provided us with exemplary care) apologised that the procedure would not be performed laparoscopically, because of the impact of COVID. My son now has a ‘vintage’ Lanz scar: a small example of how surgery which has nothing to do with COVID can nonetheless be affected.
There are also many areas beyond surgery which may be affected. Cancer referrals are one such: although two week cancer referrals have been largely maintained (largely via ‘virtual’ appointments) waiting times for surgery and treatment have inevitably been affected. Whether patients will have recourse to litigation where the waiting time is longer than it ought to be is open to question: ultimately what is reasonable during a pandemic might not be reasonable at any other time.
Evidencing the appropriate standard of care will present challenges for parties and their experts. Patients have a three-year limitation period within which to bring their claims. Lawyers and experts may well be faced with investigating a claim in, say, 2022 and will have to cast their minds back and reflect on what would have been a reasonable standard at the relevant time. Such an assessment will involve detailed factual evidence on how matters stood at the particular time in question: one can imagine defendants relying heavily on COVID policies which they might have implemented or referring to government guidance during the pandemic. And both parties will surely want to instruct experts who were in practice at the time of the crisis, so that they can speak with sufficient authority about the situation faced by medics who were ‘on the ground’ at the relevant time.
There are likely to be yet further evidential complications because of the rapid rate at which we are learning about the virus and its implications. The state of knowledge in a particular discipline is fundamental to the question of whether there has been a breach. The reasonable treatment of a COVID patient in March 2020 might be very different from treatment which might be given later that same year. These assessments (of the state of research, teaching and treatment) will be detailed and complex and, as always in clinical negligence litigation, we will depend on the quality of our experts to make such assessments.
Although the courts may be reluctant to make findings against the Health Service in the time of a pandemic, each case will be considered on its own merits. Crafting a case, or a defence, in a COVID-related clinical negligence claim is likely to be time-consuming and complicated. Just as with the virus, so with clinical negligence litigation – what we can be sure of is a period of considerable uncertainty.

On St Patrick’s Day morning this year, our youngest coughed. She coughed again. On high alert, we began a period of 14 days’ isolation during which the country was locked down. My practice, as a clinical negligence barrister, moved from being largely chambers-based to my study at home.
In spite of lockdown, and unlike colleagues in other areas of the law, I was able to continue my practice largely without interruption. Few clinical negligence cases go to trial and almost all other stages of the litigation – from the barrister’s point of view – can be dealt with remotely. Mediations and settlement meetings, in particular, seem just as successful conducted on a virtual platform.
However, many clinical negligence claims at an early stage in Spring 2020 are now subject to delay since medico-legal examinations have been difficult to organise and domiciliary visits necessarily had to be suspended during lockdown.
Claimant and defendant lawyers have largely cooperated and adopted a sensible and pragmatic approach to the challenges they face: on 14 August 2020 a new protocol was finalised between NHS Resolution, the Society of Clinical Injury Lawyers and the charity AvMA which agreed, among other things, moratoria on limitation periods until three months after the protocol ends.
Aside from the practicalities of running an existing clinical negligence claim, what are the wider implications of COVID for future clinical negligence litigation? Will there be claims by those who have contracted COVID? Probably, although the majority will likely be personal injury claims, especially employer’s liability claims for failing to provide a safe work environment and, in particular, a failure to provide adequate PPE.
Some patients may seek to bring claims against medical institutions where they have contracted COVID. In September 2020 University Hospitals Bristol and Weston NHS Foundation Trust published the findings of its investigation into a cluster of COVID deaths at Weston Hospital. The Trust apologised to the families of the 18 patients whose deaths ‘may’ have been avoided. Breach of duty in these cases may not be difficult to prove, but causation will surely be more complex, since claimants will have to prove where and how they contracted COVID and, in a fatal case, whether COVID was the cause of death. This would likely involve expert evidence from virologists and epidemiologists and, in an adversarial system, causation could be problematic (although one could imagine the doctrine of ‘material contribution’ having a role to play in some such cases).
Some of the litigation which, in the early stage of the pandemic, caused significant anxiety amongst healthcare professionals concerned the ethics of decision-making. There was a fear that doctors would be sued for their life-or-death decisions over who got a ventilator and who didn’t. Such cases would be difficult to pursue. It is a defence to a clinical negligence claim to have acted as a responsible body of your discipline would have done. So provided the actions represented those of a reasonable, responsible body of medicine and the decision-making was not illogical, there would be a defence. The courts would also, I consider, bear in mind the agony of such decision-making in a time of crisis.
It was precisely the anxiety about such claims which led to the MDU’s call, in the early days of the pandemic, for blanket immunity from clinical negligence claims for doctors in COVID times (and some US states have enacted exactly such provisions) but at present there is no indication of such legislation being enacted in the UK.
The real impact of COVID on clinical negligence claims will be on the standard of care.
Clinical negligence claims depend on the claimant proving that the relevant practitioner has fallen below a reasonable standard. It is not just doctors who owe their patients such a duty: all those involved in the running of a medical institution, from hospital porters to chief executives, have to take care when undertaking their role.
While COVID does not affect the existence of the duty, it does – and may fundamentally – affect the standard of care. This, in turn, could mean that some cases of clinical negligence are more difficult to prosecute.
In some cases the standard of care will remain unaffected: the skill with which an elective podiatry procedure is performed is likely to be judged to a similar standard in a COVID and a non-COVID world. However, emergency surgery may be affected where a hospital has COVID patients and resources have had to be diverted. In June of this year my son had appendicitis. The surgeon at Manchester Children’s Hospital (whose staff provided us with exemplary care) apologised that the procedure would not be performed laparoscopically, because of the impact of COVID. My son now has a ‘vintage’ Lanz scar: a small example of how surgery which has nothing to do with COVID can nonetheless be affected.
There are also many areas beyond surgery which may be affected. Cancer referrals are one such: although two week cancer referrals have been largely maintained (largely via ‘virtual’ appointments) waiting times for surgery and treatment have inevitably been affected. Whether patients will have recourse to litigation where the waiting time is longer than it ought to be is open to question: ultimately what is reasonable during a pandemic might not be reasonable at any other time.
Evidencing the appropriate standard of care will present challenges for parties and their experts. Patients have a three-year limitation period within which to bring their claims. Lawyers and experts may well be faced with investigating a claim in, say, 2022 and will have to cast their minds back and reflect on what would have been a reasonable standard at the relevant time. Such an assessment will involve detailed factual evidence on how matters stood at the particular time in question: one can imagine defendants relying heavily on COVID policies which they might have implemented or referring to government guidance during the pandemic. And both parties will surely want to instruct experts who were in practice at the time of the crisis, so that they can speak with sufficient authority about the situation faced by medics who were ‘on the ground’ at the relevant time.
There are likely to be yet further evidential complications because of the rapid rate at which we are learning about the virus and its implications. The state of knowledge in a particular discipline is fundamental to the question of whether there has been a breach. The reasonable treatment of a COVID patient in March 2020 might be very different from treatment which might be given later that same year. These assessments (of the state of research, teaching and treatment) will be detailed and complex and, as always in clinical negligence litigation, we will depend on the quality of our experts to make such assessments.
Although the courts may be reluctant to make findings against the Health Service in the time of a pandemic, each case will be considered on its own merits. Crafting a case, or a defence, in a COVID-related clinical negligence claim is likely to be time-consuming and complicated. Just as with the virus, so with clinical negligence litigation – what we can be sure of is a period of considerable uncertainty.

The Chair of the Bar sets out how the new government can restore the justice system
In the first of a new series, Louise Crush of Westgate Wealth considers the fundamental need for financial protection
Unlocking your aged debt to fund your tax in one easy step. By Philip N Bristow
Possibly, but many barristers are glad he did…
Mental health charity Mind BWW has received a £500 donation from drug, alcohol and DNA testing laboratory, AlphaBiolabs as part of its Giving Back campaign
The Institute of Neurotechnology & Law is thrilled to announce its inaugural essay competition
How to navigate open source evidence in an era of deepfakes. By Professor Yvonne McDermott Rees and Professor Alexa Koenig
Brie Stevens-Hoare KC and Lyndsey de Mestre KC take a look at the difficulties women encounter during the menopause, and offer some practical tips for individuals and chambers to make things easier
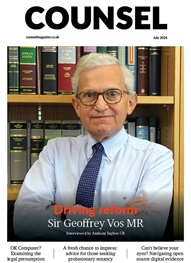
Sir Geoffrey Vos, Master of the Rolls and Head of Civil Justice since January 2021, is well known for his passion for access to justice and all things digital. Perhaps less widely known is the driven personality and wanderlust that lies behind this, as Anthony Inglese CB discovers
The Chair of the Bar sets out how the new government can restore the justice system
No-one should have to live in sub-standard accommodation, says Antony Hodari Solicitors. We are tackling the problem of bad housing with a two-pronged approach and act on behalf of tenants in both the civil and criminal courts